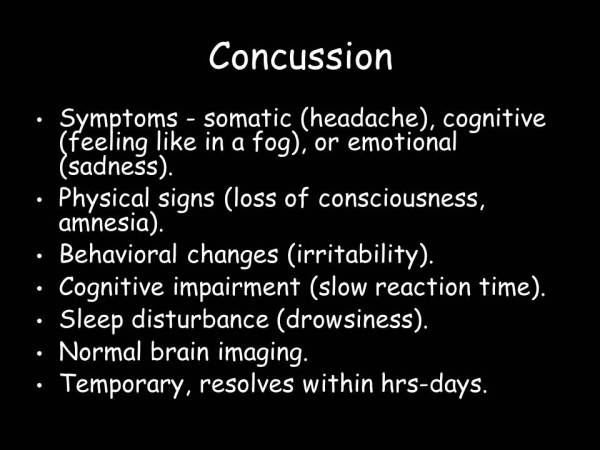
The term concussion is derived from the Latin word “concutere” which means “to shake violently”:
This term is used to describe a head injury associated with a temporary loss of brain function, including impaired consciousness, cognitive dysfunction and/or emotional problems.
xx

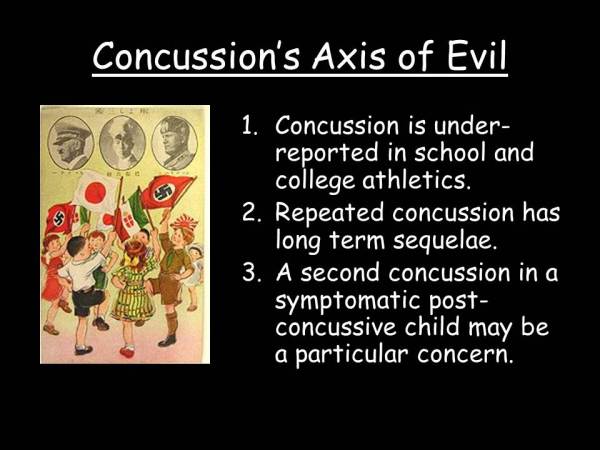
To fully understand Concussion’s Axis of Evil, one need look no further than the brutal world of professional boxing and it’s neurological complications.
xx
xx
xx
One of the most savage beatings any fighter every received occurred on July 4, 1919 in Toledo, Ohio, when 24 year old Jack Dempsey destroyed 37 year old Jess Willard to become the Heavyweight Champion of the World.
One can easily spot the effects of concussion in Willard as he sustains blow after blow to the head, and he develops unsteady gait, erratic behavior (failing to avoid punches and protect himself) and ultimately unconsciousness.
New Jersey’s own Harrison S. Martland MD (1883-1954) was the first to report in 1928 that repeated beatings of this kind could lead to a delayed permanent neurologic syndrome referred to as punch drunk syndrome.
xx
His observations went largely unheeded.
xx
Muhammad Ali (born as Cassius Marcellus Clay in 1942) was only 22 when he became word heavyweight champion in 1964, almost 40 years after Martland’s paper was published.
Here is with Liberace in 1964:
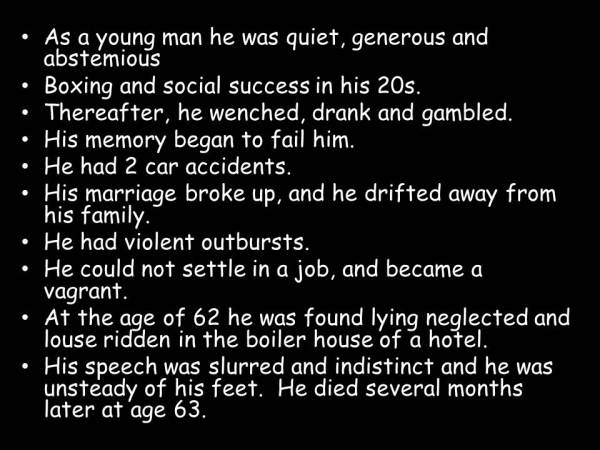
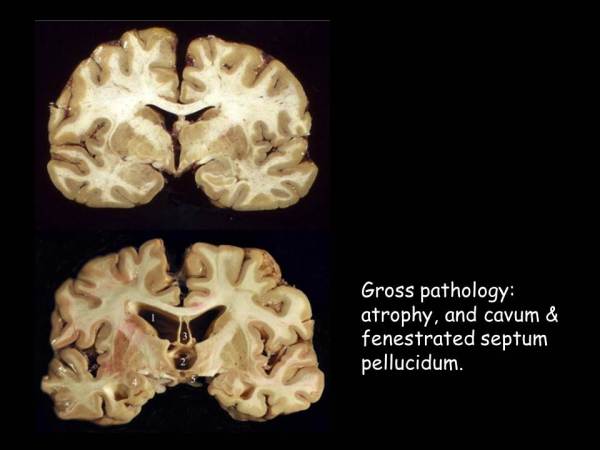
Almost 10 years after that performance, Prof Corsellis reported further clinical and pathological features of punch drunk syndrome in his 1973 paper “The Aftermath of Boxing”.
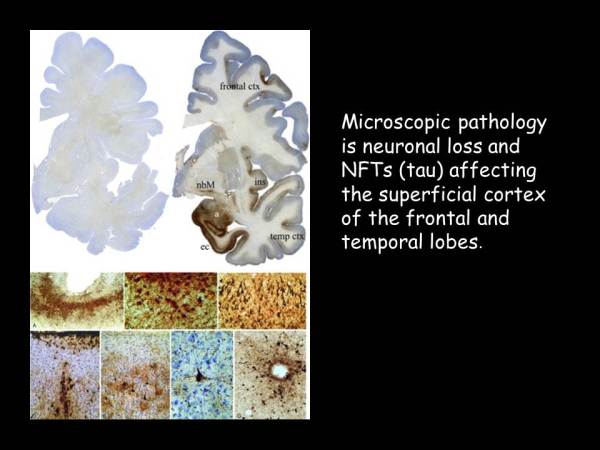
Here’s data from one of his cases:
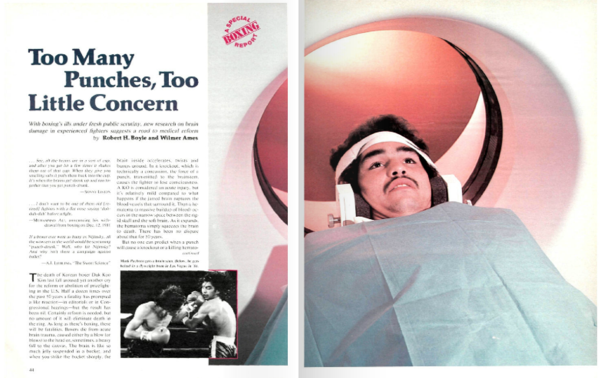
By the 1980s, reports of abnormal brain CT scans in professional boxers had reached the popular media (Sports Illustrated, 1983):
xx
By 1983, Muhammad Ali was retired from professional boxing,

and soon to be diagnosed with “Parkinson’s disease”.
xx
Here he is on the Today show with Bryant Gumbel in 1991:
Here he is in 2009:
xx
Obviously, repeated head trauma, and it’s consequences, is not unique to boxing:
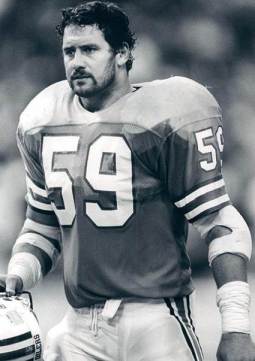 John Grimsley (1962-2008) was a linebacker for the Houston Oilers. He retired in 1993. In 2008, aged 45, he was killed by an accidental gun shout wound to the chest.
John Grimsley (1962-2008) was a linebacker for the Houston Oilers. He retired in 1993. In 2008, aged 45, he was killed by an accidental gun shout wound to the chest.
His brain was examined as part of an ongoing study by Boston University’s Study of Traumatic Encephalopathy.
xx
xx
xx
xx
xx
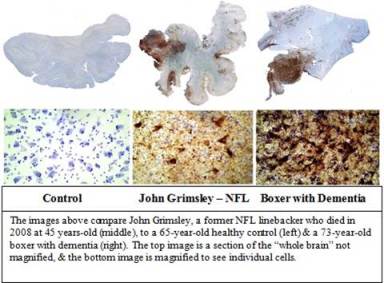 His brain showed the same pathologic changes as the Punch Drunk boxers.
His brain showed the same pathologic changes as the Punch Drunk boxers.
xx
xx
xx
xx
xx
xx
This syndrome, more commonly referred to as Chronic Traumatic Encephalopathy, is now known to have occurred as a consequence of repeated head trauma in many other sports, including soccer, hockey, horse-racing and wrestling.
College football and amateur soccer players have been shown to have impaired performance on neuropsychologic testing, worse with increasing number of concussions.
Then, there’s the Second Impact Syndrome (SIS).
SIS is said to be a rare, often fatal, traumatic brain injury that occurs when a repeat injury is sustained before symptoms of a previous head injury have resolved.
Although limited to single case reports, and disputed as a discrete syndrome in the scientific literature, SIS cases are young athletes and have become high profile in the media:

Click here to find out more about this case.
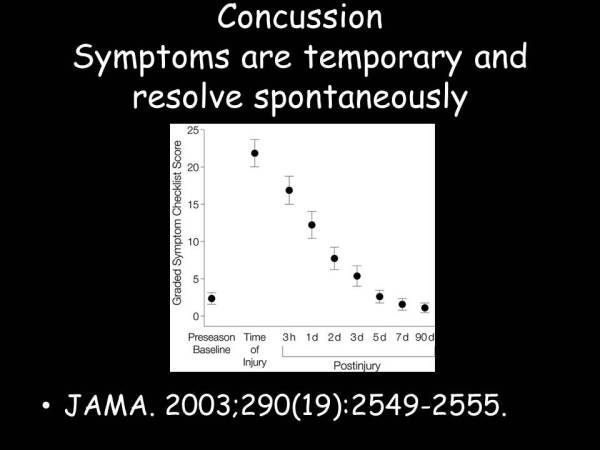
It has become clear that it takes athletes longer to recover from repeated that single concussions:
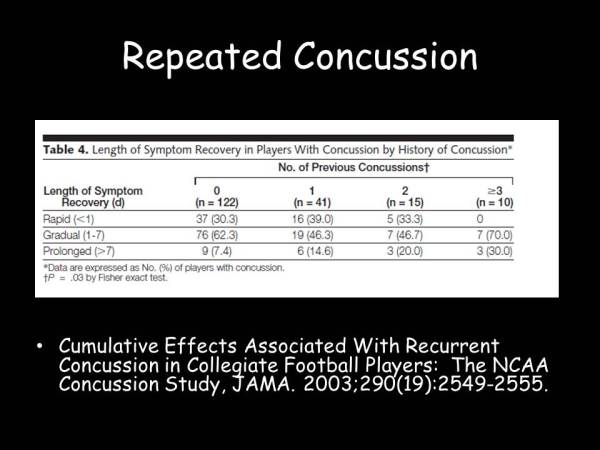
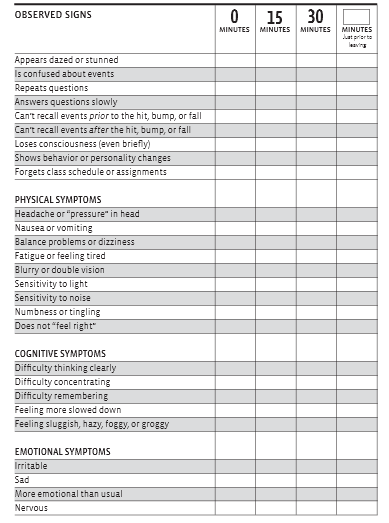
This data, as well as SIS cases, has led to a concern that the presence of ongoing concussive symptoms are a significant risk factor for further injury to occur, and that any residual symptoms should mandate restriction for further contact sport in young athletes.
xx
Finally, it is know that concussions are under-reported by high school players.
A 2004 survey of 1500 varsity football payers in Milwaukee disclosed that although 15% had sustained a concussion during the season only 50% reported it to their coach or trainer.
So there we have it, Concussion’s Axis of Evil:
xx
And the solution?
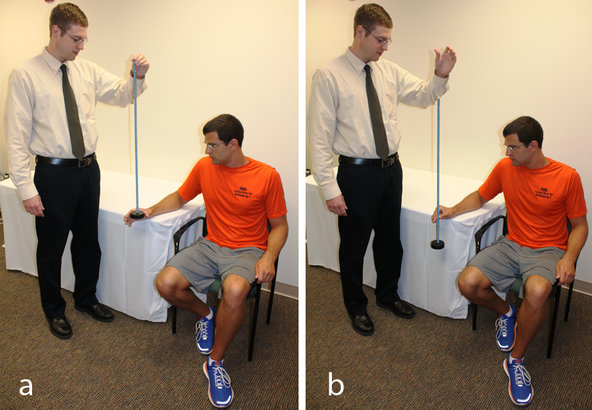
The Allies Against Concussion:
Click here to read more about how we have put these measures into effect at Monmouth Neuroscience Institute.
Click here to find out more about the Matthew J. Morahan III Health Assessment Center for athletes at Barnabas Heath.