
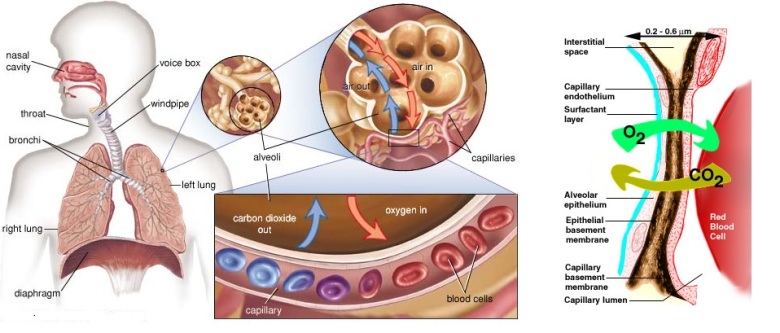
Each lung is composed of >300 million tiny membrane bound sacs of air sacs (alveoli) which if spread out would cover a piece of ground roughly the size of a tennis court. The purpose of this giant membrane is to exchange oxygen from the air for carbon dioxide from the blood stream.
xx
If the lungs become congested (or filled with fluid) from infection (pneumonia) or heart failure, it becomes harder to extract oxygen from the air:

Treatment includes adding extra oxygen to the air to make this process more efficient.
cc
However, gas exchange across the alveoli can only occur if fresh air is brought into the lungs, and stale air is moved out, a process known as ventilation. The diaphragm and muscles of the chest wall act like a giant bellows to make this happen:

These muscles can become weak in nerve or muscle diseases such as Guillain-Barré syndrome, polio, amyotrophic lateral sclerosis (ALS), Duchenne Muscular Dystrophy and myasthenia gravis.
cc
These patients are evaluated by pulmonary function testing, which will usually show a low forced vital capacity, low cough flow, and in advanced cases, elevated end-tidal carbon dioxide level.
cc
Patients with this type of ventilatory failure do not need extra oxygen, their lungs can extract oxygen from air normally, they need mechanical assistance moving air across their lungs:
cc
cc
Early neuromuscular respiratory muscle weakness causes nocturnal hypoventilation. This is because the weakened diaphragm is even more inefficient when laying supine in bed with the stomach contents pressing up on it.
Nocturnal hypoventilation presents with daytime sleepiness, early morning headaches, fatigue, and impaired cognition.
Click here to take an on-line test, and find out how sleepy you are during the day. If you score 10 or higher, you might have a problem!
Nocturnal hypoventilation is best treated using a non-invasive respirator at night, either with a face or nose mask:

cc
Other patients use a negative pressure respirator vest, or cuirass, which requires the patient to wear an upper body shell attached to a pump which actively controls the respiratory cycle:

xx
Neuromuscular respiratory failure also leads to an ineffective cough, which in turn predisposes patients to aspiration, retention of secretions, or pneumonia. Affected patients need to learn to use the cough assist machine when they get a minor respiratory tract infection to help them clear their secretions and prevent pneumonia:

xx
More severe neuromuscular ventilatory failure leads to rapid shallow breathing, accessory respiratory muscle use, thoracoabdominal paradox (inward motion of the abdomen during inspiration), and ultimately high blood levels of carbon dioxide.

Thoracoabdominal paradox – Normal (upper) abdomen moves outward with inspiration (diaphragm contraction). NM weakness (lower) abdomen moves in when patient inspires using accessory muscles.
In these cases, respiratory support is needed day and night.
Some patients can continue to use non invasive respiratory support, sleeping with a face or nose mask, and using a mouth piece intermittently during the day:

Others cannot tolerate noninvasive ventilation or have anatomic abnormalities that preclude fitting of noninvasive ventilators. Some disease, such as advanced ALS and Duchenne muscular dystrophy, affect the upper airway muscles as well as the diaphragm, impairing swallowing and compromising airway protection from aspiration. These patients can chose to be managed with invasive respiratory support using a tracheotomy and conventional ventilator.

xx
Click here and and here to find out more about the management of neuromuscular respiratory failure.

