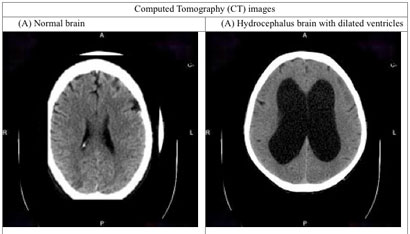
Normal pressure hydrocephalus (NPH) is caused by excessive accumulation of cerebrospinal fluid (CSF) and enlargement of the brain’s ventricular system, putting increased pressure on the surrounding brain tissue, and leading to a distinctive gait disturbance, urinary incontinence and mental decline.
NPH can be effectively treated by a surgical procedure to divert the CSF from the ventricles into the peritoneal cavity via a ventriculoperitoneal shunt. Early diagnosis and treatment are important for this surgical treatment to be effective.
However, many patients with dementia or gait problems and large ventricles on a brain imaging study will not improve after shunting. Performing surgery on all such patients, without further selection, can result in ineffective surgery, and more importantly other potential complications like bleeding around the brain (a subdural hematoma).
Therefore selecting the patients with suspected NPH who are most likely to benefit from surgery is of the utmost importance. Most patients with suspected NPH will first undergo a lumbar puncture to measure the CSF pressure, and then drain off excess fluid, temporarily lowering the pressure. If they improve after this procedure they will usually be referred for placement of a permanent ventriculoperitoneal shunt.
However, “improvement” after lumbar puncture is generally assessed subjectively, and can be very transient. Some NPH patients who do not improve after lumbar puncture do still benefit from a shunting procedure. Studies have shown that careful evaluation of patients using objective measures during prolonged CSF drainage via a lumbar drain is the most sensitive and specific way to predict which patients will improve with surgery.
The Monmouth Neuroscience Center has developed a multidisciplinary hydrocephalus assessment program to evaluate patients with suspected NPH and determine who is most likely to benefit from a shunting procedure. Patients are admitted to the intensive care unit, where a sterile lumbar drain can be placed to continuously drain CSF over 1-3 days, while they are carefully evaluated by our multidisciplinary team of neurologists, neurosurgeons and physical therapists for improvement in memory and gait using objective measures including videotaped gait analysis.
At the conclusion of the procedure, the drain is removed, and patients can review this data with their doctors to decide whether they might benefit from elective re-admission for placement of a permanent ventriculoperitoneal shunt. Our surgeons implant shunts with magnetically programmable valves allowing easy access to fine tune shunt function over time. Patients are regularly followed by our team of neurologists and neurosurgeons, with ongoing adjustment of the valve in the shunt using an external programming device to ensure the correct rate of CSF drainage, to maximize neurologic improvement and minimize complications.
Click here for more examples of neurogenic gait disorders. For more information about the NPH program at Monmouth Neuroscience Institute, please visit our website, or call us at (732) 923-5576
