Posted by David Cuthbert, MSIV, Drexel University College of Medicine
Every year thousands of people flock to several world locations with one common goal in mind – to push their bodies well beyond what nature has so far intended by climbing to dangerously high altitudes.
For whatever reason this appeals to some people. Those people are eager to overcome the restrictions set by Mother Nature, despite the obvious dangers.
As a kid I loved the move Cliffhanger with Sylvester Stallone. I remember watching that film and thinking that the only real dangers associated with extreme altitude were obvious – falling (please see video clip # 1), Slyvester Stalone wanting to use you as a human sled (watch video clip #1 again), the cold, or John Lithgow going crazy and wanting to use a helicopter to kill you for money (please see video clip #2).
But apparently those aren’t the only dangers, and medical school has taught me some pretty interesting stuff.
In fact there are a whole variety of medical syndromes that can occur at high altitude that don’t involve John Lithgow, and being that this is a neurology blog, this piece will focus on the neurological high altitude medical syndromes. And in particular, will place emphasis on one terribly interesting study.
Elevated intracranial pressure at high altitude may be a function of brain size?
The “Tight Fit Hypothesis”, and the story of one extremely curious neurosurgeon.
The neurological syndromes of high altitude sickness are thought to be a spectrum of illness ranging from high altitude headache (HAH), to acute mountain sickness (AMS), to the most severe – high altitude cerebral edema (HACE).
The exact pathophysiologic mechanisms leading to these conditions are still somewhat unclear but several theories have been proposed and tested – all of which related to hypoxia and elevated intracranial pressure (ICP).
It is thought that in the milder end of this spectrum (HAH) the symptoms are solely contributed from hypoxia, and as disease severity progresses, and the patient comes closer to HACE – the pathogenesis is more attributable to raised ICP.
But what I find even more interesting than just the development of these syndromes – is the fact that there is great variability between who develops them. For some people, no matter how acclimatized they are they simply cannot go to a certain altitude without great risk of HACE and subsequent death. While others require little acclimatization, and are capable to trekking to the summit of Mt. Everest without necessitating the use of supplemental oxygen. This leads one to ask, what are the factors present that allow someone this ability to tolerate high altitude?
One answer (with considerable evidence to support it) lies within their genetics. The discovery of a transcription factor called “Hypoxia Inducible Factor”, or HIF, confirmed this. HIF is a transcription factor that contributes to the regulation of several metabolic pathways, and allows both production of a higher concentration of hemoglobin, and greater sensitivity of the carotid body to hypoxia. Another older, and forgotten theory looks to further explain this increased altitude tolerance through anatomic differences.
In 1985 Ross suggested that the “random nature of cerebral mountain sickness” can be explained by “more compliant systems”. In other words, if a person has larger sized ventricles, and/or more atrophic brain, they will in turn be less susceptible to altitude sickness because the compliance will leave them better equipped to tolerate the raise intracranial pressure.
Interestingly enough, there existed someone crazy enough to test this hypothesis. Someone not only willing to hike to these ungodly altitudes, but also willing to screw a bolt in his head to measure his own intracranial pressure. This person was Brian Cummings, an avid outdoorsman, who also just so happened to be a neurosurgeon.
Cummings and a team of ten undertook an expedition to the Kishtwar region of northern India to try to put this hypothesis to the test. However the data obtained from the experiment was destroyed in a fire. Or so everyone thought! Then recently Cummings wife (Cummings has since passed away) found the data from the experiment, allowing it to have since be published.
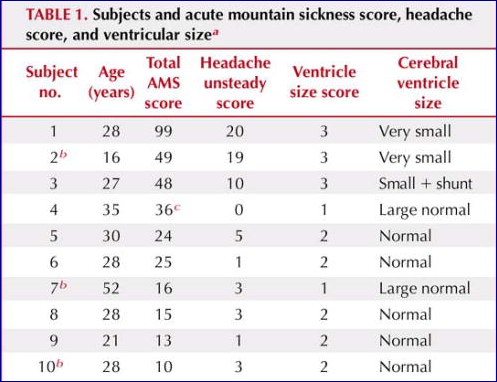
In this experiment the “tight fit” hypothesis was tested by using 10 subjects. These subjects had computed tomographic scans of their brains to measure their ventricular size. After which a scoring system was used to measure symptomatology related to high altitude neurological syndromes while at high altitudes. Also, three lucky volunteers had their intracranial pressures measured – allowed via screwing a pressure monitor through a burr hole in their heads . This stayed in place while trekking through Northern India Himalaya’s. Cummings himself participated in the study, and also had a pressure monitor placed.
The results of the study showed that the three subjects with the smallest ventricles suffered the most from Acute Mountain Sickness, and reported the worst headaches of the group. Meanwhile patients with larger to normal sized ventricles reportedly had significantly less clinical findings related to AMS:
Regarding the intracranial pressure monitoring, of the 3 subjects to be observed, one had large ventricles, one with normal size, and one with small ventricles. The only one to experience headache, was the patient with the highest observed rise in ICP, and was also the subject with the smallest ventricles.
Therefore the results of this experiment support Ross’s “tight fit” hypothesis, and provide a potential anatomic explanation to compliment other genetic mechanisms to explain why some people are more prone to developing high altitude neurologic syndromes.
Obviously, the small study size cannot definitively explain this susceptibility, nor can it exclude other mechanisms as contributing as well. Nevertheless this experiment is considerably important to those who wish to conquer the hypoxic environment of Mother Nature’s higher altitudes.
It allows an explanation for those that are less able to adapt, and maybe even one day provide a means of testing their ability to acclimatize prior to their summit attempt. And while that very well may never happen, this study at the very least is a great story about the incredible strength of the human spirit.
Dr. Cummings showed incredibly determination while searching for answers regarding the human ability to adapt to their environment, and fortunately now his work can live on.



I find this article quite interesting since I live at 10,000 feet in the rocky mountains. I have to say that I’ve witnessed first hand that lower oxygen levels have tremendous impacts on people and their health and mental stability.
The most significant contributing factors to hypoxia I’ve found are incorrect foods for the blood type and low alkalinity levels in the blood. The low alkalinity levels are due mainly to improper foods for their blood type, often aggravated by the regular use of tobacco, alcohol or prescription drugs.
After what I’ve witnessed and after reading the article… it makes me wonder whether the small ventricle subjects were all of the same blood type? Perhaps having negative reactions to the food that the other blood types were eating without that type of reaction?
Just postulating here. 🙂
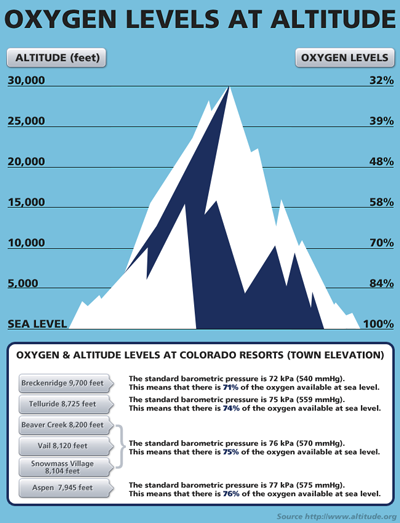
Anyway, thanks for posting an interesting article on the subject… I had no idea I was dealing with 70% oxygen levels as compared to sea level. Certainly explains a lot. 🙂
Keep it Clean