Post prepared by Precious Ramirez-Arao, Monmouth Medical Center PGY3
A 60 year-old female was found lethargic lying in a pool of feces by roommate.
EMS was called and was immediately brought to the hospital.
In the emergency department she had a witnessed generalized tonic-clonic seizure.
Her roommate relates she had episodes of confusion and short-term memory loss over the past few weeks.
She remained lethargic over the next 72 hours in the hospital.
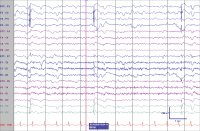
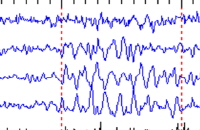
48-hour EEG monitoring showed diffuse 2 to 3 Hz delta slowing with periodic lateralized epileptiform discharges emanating from the left frontal temporal region.
T2 weighted image of the brain showed signal abnormality of the left mesial temporal lobe and the pulvinar with diffusion restriction in the left hippocampus consistent with limbic encephalitis.
Limbic encephalitis (LE) is a subacute syndrome of seizures, personality change and cognitive dysfunction, typically evolving over days to weeks.
Autoimmune and paraneoplastic forms have been described. The most common neoplasms associated with paraneoplastic LE are lung cancer (usually small cell), thymoma, ovarian or testicular teratoma, breast cancer and Hodgkin lymphoma. The associated autoantibody depends on the tumor type. Lung cancer and thymomas are associated with anti-VGKC while ovarian or testicular teratomas are associated with antiNMDA antibodies.
Neurologic symptoms can precede oncologic diagnosis for several months to years and initial CT scans are typically unrevealing.
Nevertheless, prompt and thorough evaluation for malignancy including PET and CT scan of the chest, abdomen and pelvis should be initiated. Symptomatic treatment includes corticosteroids, plasmapharesis and intravenous immune globulin.







 The National Association of Epilepsy Centers (NAEC)
The National Association of Epilepsy Centers (NAEC)

